Growth hormone (GH) is a vital player in the human body, influencing everything from childhood development to adult metabolism. But sometimes, the production of this essential hormone can falter, leading to a condition known as growth hormone deficiency (GHD).
This condition can be a source of concern, particularly for parents of children experiencing stunted growth. However, in Pakistan, there’s no need to despair! We have access to a range of resources and treatment options to address GHD effectively.
This blog post serves as your one-stop guide to growth hormone deficiency in Pakistan. We’ll explore the signs and symptoms you might encounter, the treatment options available, and the medications used to manage this condition. By the end, you’ll be well-equipped with knowledge about GHD, its impact on health, and the resources available to address it here in Pakistan.
What is Human Growth Hormone Deficiency?
Human growth hormone (HGH) deficiency is a condition where the pituitary gland, located at the base of the brain, doesn’t produce enough HGH. HGH is a crucial hormone that plays a vital role in regulating growth, development, and metabolism throughout your life.
What are the Causes of the Growth Hormone Deficiency?
While the exact cause can vary, here’s a breakdown of the two main categories of growth hormone deficiency:
Congenital Growth Hormone Deficiency (Present from Birth):
Genetic Mutations: In some cases, genetic mutations can affect the pituitary gland or the genes responsible for HGH production. These mutations can be inherited from parents or occur spontaneously.
Pituitary Gland Malformations: Sometimes, the pituitary gland itself may develop abnormally, hindering its ability to produce sufficient HGH. This can occur during fetal development.
Complications During Childbirth: Difficult or traumatic childbirth can, in rare cases, damage the pituitary gland and impact HGH production.
Acquired Growth Hormone Deficiency (Develops Later in Life):
Injury: Head trauma or injury to the pituitary gland can disrupt its function and lead to HGH deficiency.
Infection: Certain infections, such as meningitis or encephalitis, can damage the pituitary gland and affect HGH production.
Tumor: A tumor in the pituitary gland or surrounding area can put pressure on the gland, affecting its ability to produce HGH.
Radiation Treatment: Radiation therapy to the head or neck for cancer treatment can sometimes damage the pituitary gland and cause HGH deficiency.
Autoimmune Disease: In rare cases, an autoimmune condition can attack the pituitary gland, leading to HGH deficiency.
What are the Signs of Growth Hormone Deficiency?
The signs of growth hormone deficiency occur mostly in children, but it can happen in adults as well. here’s a breakdown of the signs to watch for in both children and adults.
Signs in Children (Most Common During Diagnosis):
Slow Growth Rate: This is a primary indicator. Your child might be consistently falling below the expected growth percentiles on a growth chart.
Delayed Puberty: Children with HGH deficiency may experience a delay in the onset of puberty, such as breast development in girls or testicular enlargement in boys.
Short Stature Compared to Peers: Children with HGH deficiency are often significantly shorter than their peers of the same age and sex.
Decreased Muscle Mass and Increased Fat Stores: HGH helps build muscle and burn fat. A deficiency can lead to a lean body with less muscle and a higher percentage of body fat.
Low Energy Levels and Fatigue: Children with HGH deficiency may often appear tired and lack the energy levels of their peers.
How Common is Growth Hormone Deficiency?
Growth hormone deficiency is a relatively rare condition. Here’s a look at its estimated occurrence:
Children: Studies suggest that about 1 in 3,500 to 10,000 children have congenital growth hormone deficiency. This means for every 3,500 to 10,000 children born, approximately one might have this condition.
Adults: The exact prevalence of HGH deficiency in adults is unknown, but it’s likely less common than in children. Diagnosing adult-onset HGH deficiency can be challenging due to the subtlety of symptoms, making it difficult to determine precise figures.
How to Test Your Growth Hormone Deficiency?
While there’s no single definitive test for HGH deficiency, several assessments can help your doctor make a diagnosis. Here are some common approaches:
Blood Tests: These tests measure your IGF-1 (insulin-like growth factor 1) levels. IGF-1 is a hormone produced by the liver in response to HGH stimulation. Low IGF-1 levels can indicate HGH deficiency. However, other factors can also affect IGF-1, so additional tests might be needed.
Growth Hormone Stimulation Tests: These tests involve measuring your HGH levels in your blood after stimulation with certain substances like medications or specific amino acids. There are different types of stimulation tests, and your doctor will choose the most appropriate one for you.
Imaging Tests: In some cases, an MRI scan of the pituitary gland might be recommended to check for any abnormalities in its structure that could be hindering HGH production.
What Happens If you have a Growth Hormone Deficiency?
Growth hormone deficiency is a treatable condition. With proper diagnosis and treatment, individuals with HGH deficiency can experience significant improvements in growth, development, and overall well-being.
If you suspect you or your child might have HGH deficiency, consulting a healthcare professional is crucial. Early diagnosis and treatment can help prevent or minimize the potential consequences of this condition.
What are the Treatments of Growth Hormone Deficiency?
The growth hormone deficiency treatment has multiple options available to address this condition. Here’s a breakdown of the primary approach:
Treatment with Synthetic HGH:
The mainstay of treatment for HGH deficiency is injections of synthetic HGH. These injections replicate the effects of naturally produced HGH and can significantly improve symptoms.
Treatment is typically administered daily and requires ongoing monitoring by a healthcare professional.
Dosage is individualized based on factors like your age, severity of deficiency, and treatment goals.
What are the Injections Available for Growth Hormone Deficiency?
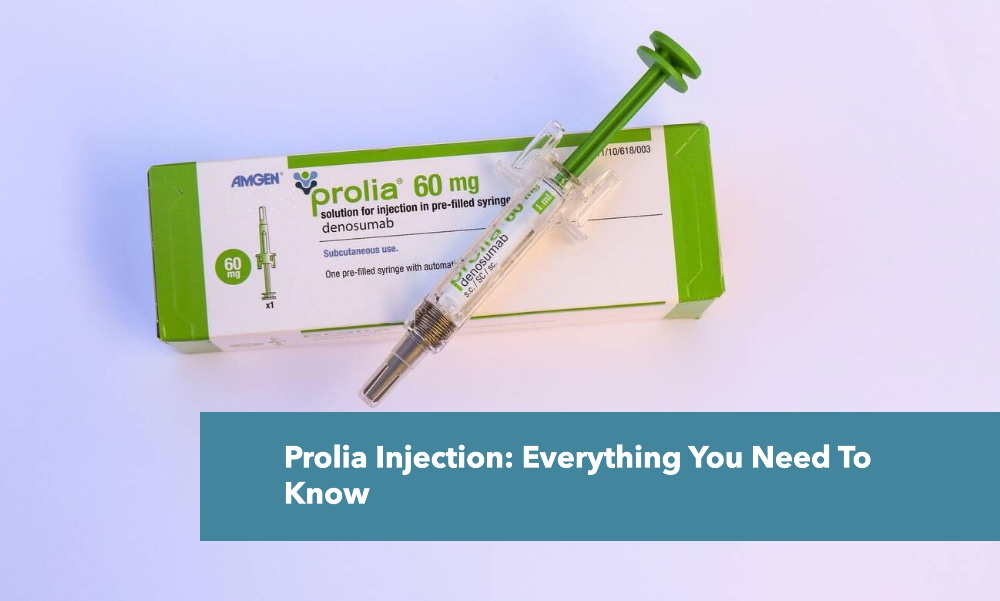
There are several different brands of HGH injections available in Pakistan. Some common brands include:
Genotropin
Humatrope
Norditropin
Saizen
Protropin
What Happens if Growth Hormone is Not Treated?
While not life-threatening itself, untreated HGH deficiency can lead to various health complications that can significantly impact your well-being. Here’s a breakdown of the potential consequences for children and adults.
Delayed Puberty: HGH also plays a role in triggering the hormonal changes associated with puberty. Children with untreated HGH deficiency may experience a significant delay in the onset of puberty.
Decreased Muscle Mass and Increased Fat Stores: HGH helps build muscle and burn fat. Untreated deficiency can lead to a lean body with less muscle and a higher percentage of body fat.
Reduced Bone Density: HGH is essential for building strong bones. Untreated deficiency can lead to weaker bones and an increased risk of fractures in children.
Delayed Development: HGH deficiency can also impact cognitive development and motor skills in children.
Is Growth Hormone Treatment Curable?
While there isn’t a permanent “cure” that completely restores natural HGH production, effective treatments can significantly improve symptoms and overall health. Here’s a breakdown of what you can expect:
Management Through Treatment:
The primary treatment for HGH deficiency is injections of synthetic HGH. These injections replicate the effects of naturally produced HGH and can significantly improve symptoms.
HGH therapy is a long-term commitment, typically lasting for several years or even a lifetime. Regular monitoring by a healthcare professional is crucial to ensure optimal treatment and address any potential side effects.