Exocrine pancreatic insufficiency (EPI) is a digestive disorder that occurs when your pancreas doesn’t make enough of the enzymes you need to digest food properly. The pancreas is a gland located behind your stomach that releases enzymes into your small intestine to help break down carbohydrates, proteins, and fats in the food you eat.
What is an Exocrine Pancreatic Insufficiency?
Exocrine Pancreatic Insufficiency, or EPI, is a digestive disorder that affects how your body breaks down food. Normally, your pancreas makes enzymes that act like tiny scissors, chopping your food into small pieces so your body can absorb the nutrients.
In EPI, your pancreas doesn’t make enough of these enzymes, or the ones it produces aren’t strong enough. This means food isn’t broken down properly, and nutrients like fats, proteins, and carbohydrates can’t be absorbed well.
Symptoms and Causes
What Causes Exocrine Pancreatic Insufficiency?
Exocrine Pancreatic Insufficiency (EPI) develops when your pancreas, a gland behind your stomach, isn’t producing enough digestive enzymes. These enzymes are like tiny helpers in your digestive system, breaking down food into smaller pieces so your body can absorb the nutrients it needs.
So, what can cause this lack of enzymes? Here are some of the most common reasons:
Chronic Pancreatitis: This is an inflammation of the pancreas that lasts for a long time. Repeated inflammation can damage the pancreas and reduce its ability to make enzymes.
Cystic Fibrosis: This genetic condition affects many organs, including the pancreas. In cystic fibrosis, thick mucus builds up in the pancreas, blocking the enzymes from reaching your intestines.
Surgery: If you’ve had surgery on your pancreas, it can sometimes damage the tissue responsible for enzyme production.
Other health conditions: In rare cases, autoimmune diseases or certain medications can harm the pancreas and lead to EPI.
What Causes Exocrine Pancreatic Insufficiency in Children?
Exocrine Pancreatic Insufficiency (EPI) in children happens when their pancreas isn’t making enough digestive enzymes. These enzymes, like tiny helpers, break down food into pieces their bodies can absorb nutrients from.
Several conditions can cause EPI in children, some more common than others:
Cystic Fibrosis: This genetic condition is the leading cause of EPI in children. It causes thick mucus to build up in many organs, including the pancreas. This mucus blocks the enzymes from reaching the intestines, where they’d normally help digest food.
Shwachman-Diamond Syndrome (SDS): This is another genetic condition that affects the pancreas. In SDS, the part of the pancreas that makes enzymes doesn’t work properly.
Other, less common causes of EPI in children include:
Chronic pancreatitis: This is inflammation of the pancreas that lasts a long time. It’s rare in children, but it can damage the pancreas and reduce enzyme production.
Pancreatic agenesis/hypoplasia: In rare cases, a child might be born missing part or all of their pancreas (agenesis) or have an underdeveloped pancreas (hypoplasia).
Isolted enzyme deficiencies: Sometimes, a child might have a problem with just one specific digestive enzyme, not all of them.
What Causes Exocrine Pancreatic Insufficiency in Adults?
Exocrine Pancreatic Insufficiency (EPI) in adults develops when your pancreas, a digestive gland behind your stomach, doesn’t make enough digestive enzymes.
EPI contributing to diabetes: In rare cases, EPI can indirectly lead to diabetes. When your body can’t absorb nutrients properly due to EPI, it can affect how your body regulates blood sugar. This can contribute to problems like insulin resistance, a precursor to type 2 diabetes
Chronic Pancreatitis: This is the leading culprit behind EPI in adults. It involves long-term inflammation of the pancreas, which can scare and damage the tissue responsible for enzyme production. The most frequent causes of chronic pancreatitis are heavy alcohol consumption and smoking, but sometimes the exact cause remains unknown.
Surgery: If you’ve undergone pancreatic surgery, such as for gallstones or tumors, it can potentially affect your enzyme production. The amount of remaining pancreatic tissue and its functionality will determine if EPI develops.
Cystic Fibrosis: While typically diagnosed in childhood, some adults might not be diagnosed with cystic fibrosis until later in life. This genetic condition causes thick mucus to build up in the pancreas, blocking the enzymes from reaching your intestines for digestion.
What are the Symptoms of Exocrine Pancreatic Insufficiency (EPI )?
Several signs and symptoms can indicate EPI in adults. Here are the most common ones:
Digestive Discomfort: After eating, you might experience bloating, cramps, or pain in your belly. This discomfort happens because undigested food irritates your intestines.
Frequent Diarrhea: You might have frequent loose, oily stools that float due to the presence of undigested fats. This is because your body can’t absorb these fats properly without enough enzymes.
Weight Loss: Even though you might be eating enough, you could experience unexplained weight loss. This happens because your body isn’t absorbing the nutrients it needs from food due to the lack of enzymes.
Fatigue: Feeling tired and run down can be a sign that your body isn’t getting the energy it needs from food because of EPI.
Other possible symptoms of EPI in adults include:
- Vitamin deficiencies: Since EPI affects nutrient absorption, you might develop deficiencies in vitamins A, D, E, and K.
- Pale, greasy stools
- Increased gas
It’s important to remember that these symptoms can also be caused by other conditions. If you’re experiencing any of these issues, talking to your doctor is crucial for proper diagnosis.
What are the first signs of Exocrine Pancreatic Insufficiency (EPI )?
Here’s what to watch out for in the early stages of EPI:
Changes in Your Stool: This is often the first clue that something might be amiss. You might notice:
Increased Stool Frequency: You might have to go to the bathroom more often than usual.
Loose Stools: Your stools might become looser or more watery than usual.
Oily or Greasy Stools: Undigested fats can make your stools appear oily or greasy. They might also float in the toilet bowl.
Mild Abdominal Discomfort: After eating, you might experience:
Bloating: You might feel uncomfortably full or swollen in your belly.
Cramps: You might have mild cramping or aching in your abdomen.
Unexplained Weight Loss: Even though you might be eating enough, you could start losing weight unintentionally. This happens because your body isn’t absorbing nutrients properly due to the lack of enzymes.
Diagnose and Tests:
How is exocrine pancreatic insufficiency (EPI) diagnosed?
EPI often involves a combination of tests to get a clear picture of what’s happening.
Talking to Your Doctor: They’ll start by asking you about your medical history, including any digestive problems you’re experiencing.
They’ll also want to know about any risk factors for EPI, such as chronic pancreatitis, cystic fibrosis, or previous pancreatic surgery.
Stool Tests: These are often the first tests used to check for EPI.
There are two main types:
Fecal Elastase Test: This test measures the amount of elastase, a digestive enzyme, in your stool. Low levels of elastase can indicate EPI.
Fecal Fat Test: This test measures the amount of fat in your stool. Undigested fats due to EPI can show up at higher levels.
Blood Tests: While not a direct test for EPI, blood tests can help identify other conditions that might be causing your symptoms or check for vitamin deficiencies that can arise due to EPI.
Management and Treatment:
What are the complications of exocrine pancreatic insufficiency (EPI)?
Here’s a look at some potential consequences of EPI:
Malnutrition: This is the main concern with EPI. Because your body can’t absorb nutrients properly, you might develop deficiencies in essential vitamins, minerals, and protein. This can lead to health problems like fatigue, muscle weakness, and a weakened immune system.
Weight Loss: Even if you’re eating enough, you might experience unexplained weight loss due to malabsorption of nutrients.
Growth Problems in Children: In children with EPI, malabsorption can hinder their growth and development.
Bone Problems: Vitamin D deficiency, a common complication of EPI, can lead to weakened bones and an increased risk of osteoporosis.
Other Health Issues: EPI can also increase your risk for other health problems, such as:
- Kidney stones due to increased calcium levels in the blood
- Anemia due to iron deficiency
- Increased risk of infections due to a weakened immune system
How is exocrine pancreatic insufficiency (EPI) treated?
There are effective treatments to manage EPI and improve your quality of life.
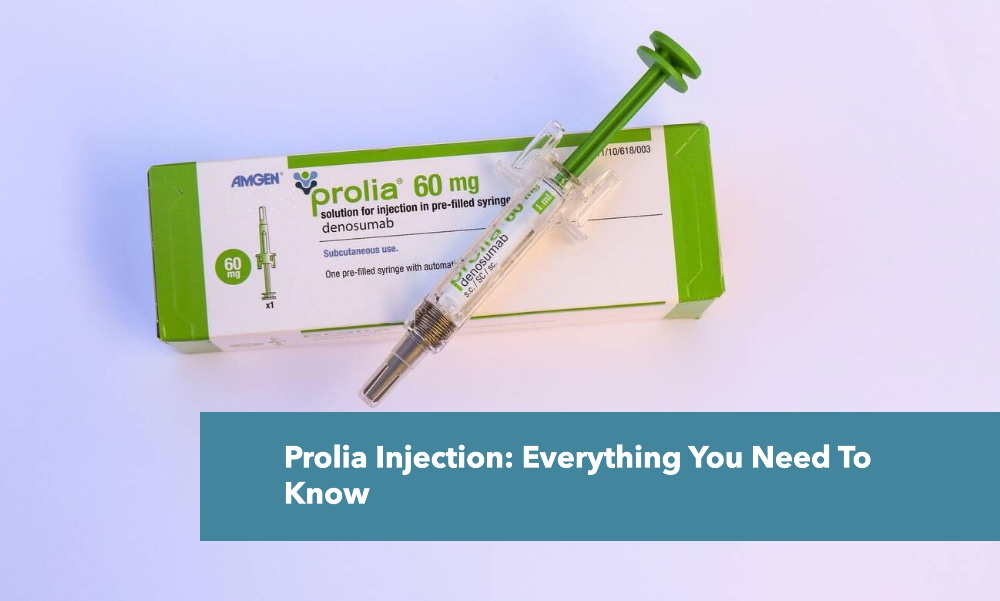
Pancreatic Enzyme Replacement Therapy (PERT): PERT involves taking capsules or tablets containing digestive enzymes with every meal and snack. These enzymes replace the ones your pancreas isn’t making, helping your body break down food and absorb nutrients.
The dosage of PERT will be determined by your doctor based on the severity of your EPI and your individual needs.
Dietary Changes: Working with a dietitian can help you create a healthy eating plan that’s easier for your body to digest.
Eating smaller, more frequent meals: This can help reduce the workload on your digestive system.
Choosing easily digestible foods: Opt for cooked over raw vegetables, lean protein sources, and healthy fats.
Limiting fatty foods: Fat can be more difficult to digest for people with EPI.
Staying hydrated: Drinking plenty of fluids is important to prevent constipation, a common side effect of EPI.
Vitamin and Mineral Supplements: Because EPI can affect nutrient absorption, your doctor might recommend supplements to address any deficiencies. These might include:
Vitamin A, D, E, and K: These fat-soluble vitamins require digestive enzymes for proper absorption.
Vitamin B12 and iron: Deficiencies in these can occur due to EPI and lead to fatigue and other health problems.
What is the medication for pancreatic enzyme deficiency?
KREON® (pancrelipase): This is a prescription medication containing a combination of enzymes similar to those your pancreas would normally make. It replaces the missing enzymes and helps your body digest food properly.
Prevention and Outlook:
How Can I Prevent Exocrine pancreatic insufficiency (EPI)?
We can focus on strategies to reduce your risk of developing conditions that can lead to EPI, such as chronic pancreatitis. Here’s what you can do:
Limit Alcohol Consumption: Heavy alcohol use is a major risk factor for chronic pancreatitis, which can eventually lead to EPI. If you drink alcohol, do so in moderation.
Say No to Smoking: Smoking can irritate the pancreas and increase your risk of pancreatitis. Quitting smoking is one of the best things you can do for your overall health, including your pancreas.
Maintain a Healthy Weight: Obesity can put stress on your pancreas. Maintaining a healthy weight through a balanced diet and regular exercise can help reduce your risk of pancreatitis.
Eat a Balanced Diet: A healthy diet rich in fruits, vegetables, and whole grains provides your body with the nutrients it needs to function properly. This can help keep your pancreas healthy.
Limit Fatty Foods: A diet high in saturated and unhealthy fats can stress your pancreas. Opt for lean protein sources and healthy fats like those found in avocados and olive oil.
What is the prognosis (outlook) for people who have exocrine pancreatic insufficiency (EPI)?
The outlook for EPI is good with early diagnosis and treatment. Sticking to your doctor’s plan (enzyme replacement, diet changes, vitamins) is key to preventing malnutrition and other complications. Regular checkups help monitor EPI and adjust treatment as needed. Talk to your doctor for any questions or concerns, and remember, you can live well with EPI.