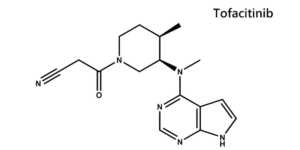
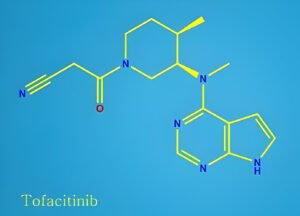
What is the Tofacitinib?
Tofacitinib is a medication doctors prescribe to help people with certain types of swelling and pain in their joints and other parts of their body. It’s a special kind of drug called a Janus Kinase (JAK) inhibitor. You can take it as a pill or a liquid, and it’s sold under the names Xeljanz and Xeljanz XR.
Doctors recommend Tofacitinib for adults who tried other treatments that didn’t work for them. It helps with:
- Really bad rheumatoid arthritis
- Psoriatic arthritis that’s active
- Ankylosing spondylitis that’s active
- Really bad ulcerative colitis
- A type of arthritis in kids over 2 years old called active polyarticular course juvenile idiopathic arthritis
It’s also for kids aged 2 to 17 years with the same type of arthritis mentioned last.
How Does Tofacitinib Work?
Tofacitinib helps people with certain arthritis types by targeting and blocking special proteins in the body called Janus Kinase (JAK) enzymes. These proteins play a big part in causing arthritis symptoms because they help send signals that lead to inflammation and pain.
When Tofacitinib stops these proteins from working, it also stops a series of steps (known as the JAK-STAT signalling pathway) that normally help the body’s immune cells react to inflammation. This means it can help control how genes work to cause inflammation, how new blood cells are made, and how immune cells behave.
By doing this, Tofacitinib helps lower the body’s reaction to inflammation. For people with rheumatoid arthritis, it can quickly lower the levels of C-reactive protein (CRP) in their blood, which is a sign that there’s less inflammation in the body.
How to Use Tofacitinib Tablet?
Tofacitinib comes in tablets you swallow by mouth. We typically start with two tablets a day, but your doctor might adjust this to just one depending on your situation.
There’s also a version called Xeljanz XR, which lasts longer in your body (extended-release). With this one, you usually only need one tablet each day. Remember to swallow these tablets whole – don’t break, crush, or chew them.
Tofacitinib works well with or without food, so take it whichever way feels best for you. If you miss a dose, don’t worry! Just take it as soon as you remember. But if it’s close to the time for your next dose, skip the missed one and get back on track with your regular schedule. There’s no need to take extra tablets to make up for a missed dose.
For children two years and older, Tofacitinib also comes as an easy-to-swallow liquid.
What are the Side Effects of Tofacitinib?
Tofacitinib can cause some side effects. Let’s talk about the most common ones first: these are usually mild, like headaches, diarrhea, stuffy nose, and sore throat.
There are also more serious side effects to be aware of. Here’s what to watch for:
- Infections: Tofacitinib can make it harder for your body to fight off infections, including tuberculosis (TB).
- Cancer: There’s a chance it could increase your risk of certain cancers, especially if you smoke.
- Heart problems: If you have risk factors for heart disease, Tofacitinib might raise your chances of having a heart attack, stroke, or other serious heart problems.
- Blood clots: These can form in your lungs, legs, arms, or even arteries.
- Tears in your stomach or intestines: This is more likely if you also take NSAIDs or corticosteroids.
- Allergic reactions: These can cause swelling in your lips, tongue, or throat, or give you hives.
- Liver and cholesterol changes: Your doctor will monitor these with routine tests.
- Reduced fertility: Tofacitinib might affect fertility in women of child-bearing age. It’s unclear if this is permanent.
Seek Urgent Medical Attention if you Experience Any of These:
- Chest pain, tightness, or discomfort
- Shortness of breath
- Pain radiating to your arms, nerve pain, back pain, neck, or jaw
- Cold sweats
- Weakness on one side of your body
- Sudden trouble breathing
- Leg pain, swelling, redness, or tenderness
- Signs of an allergic reaction (swelling, hives)
What are the Warning and Precautions of Tofacitinib?
Tofacitinib is a powerful medication, and there are some things to consider before you start taking it. Let’s go through them together:
- Infections: Tofacitinib can make it harder for your body to fight off infections, especially if you’re already taking medications that suppress your immune system. Be sure to tell your doctor if you have any signs of infection before starting or while taking Tofacitinib.
- Increased Death Risk: Studies have shown a higher risk of death in people over 50 who take the higher dose of Tofacitinib. Your doctor will discuss this risk with you and determine the best dosage.
- Blood Clots: There’s an increased chance of blood clots, especially if you’re over 50 and have risk factors for heart disease. Talk to your doctor about this.
- Cancer: There have been reports of lymphoma, skin cancer, and other cancers in people using Tofacitinib. Tell your doctor if you’ve had any previous cancers.
- Liver Problems: If you have severe liver problems, Tofacitinib is not for you.
- Kidney Transplants: Tofacitinib is not recommended for people who have had a kidney transplant.
- Other Considerations: Tofacitinib may not be suitable if you have a low white blood cell count, are pregnant, breastfeeding, or over 65. It’s also important to avoid taking Tofacitinib with other medications that suppress your immune system.
- Side Effects: Tofacitinib may raise your cholesterol levels and affect liver function tests. Your doctor will monitor these with regular checkups.
- Weakened Immune System: Since Tofacitinib affects your immune system, it’s wise to avoid close contact with people who are sick.
- Vaccinations: Tell your doctor if you need any vaccinations and make sure all your vaccinations are up-to-date before starting Tofacitinib. You should avoid live vaccines while on this medication.
How Does Tofacitinib Interact with Other Medicines?
Tofacitinib can interact with certain medications, so it’s important to tell your doctor about everything you’re taking, including prescriptions, over-the-counter meds, and herbal supplements. Here are some examples:
- Immunosuppressants: These medications also weaken your immune system, so taking them with Tofacitinib could put you at higher risk of infections. Examples include abatacept, adalimumab, and anakinra.
- Certain antifungals and antibiotics: Medications like ketoconazole, fluconazole, and rifampin can affect how your body processes Tofacitinib.
- Other medications: Tofacitinib may also interact with arthritis medications (NSAIDs), seizure medications, steroids, St. John’s Wort, and some cholesterol medications.
Important Safety Reminders:
- Don’t take Tofacitinib with strong immunosuppressants.
- Tell your doctor about any infections before starting Tofacitinib. They may need to test you for tuberculosis (TB) before you begin treatment.List of Complete Medications which are frequently checked.
Your doctor will consider all your medications and health conditions to determine if Tofacitinib is right for you. Be sure to disclose everything you’re taking to ensure safe and effective treatment.
What Happens if I Miss a Dose of Tofacitinib?
If you miss a dose of tofacitinib, take it as soon as you remember. However, if it’s nearly time for your next dose simply skip the missed dose and continue with your normal routine. Don’t take a double dose to make up for a missed one.
What Happens if I Overdose on Tofacitinib?
Tofacitinib overdose is a serious situation. Unlike some medications, there isn’t a specific antidote for Tofacitinib. If you think you or someone you know has taken too much, it’s vital to take immediate action.
Here’s What to do:
- Call emergency services or your local poison control center right away. Don’t wait for symptoms to appear.
- They will likely advise you to monitor the person for any signs of serious side effects. These can be similar to the medication’s known side effects, but more severe.
Be Aware of Potential Symptoms:
Infections, especially tuberculosis
Heart problems like heart attack or stroke (more likely in people over 50)
Liver problems (dark urine, yellowing of skin/eyes, stomach pain)
Remember: Getting medical attention as soon as possible is crucial in an overdose situation. Every minute counts.