What is a Fingolimod?
Fingolimod is a medication used to treat relapsing-remitting forms of multiple sclerosis (MS). It falls under the category of sphingosine 1-phosphate receptor modulators.
Relapsing-remitting MS is a progressive condition where symptoms flare up (relapses) followed by periods of partial or complete recovery. Fingolimod doesn’t cure MS, but it helps manage the disease by:
Reducing Relapses: Studies suggest it can significantly decrease the frequency of relapses.
Slowing Progression: It may help slow down the worsening of disability associated with MS.
What is the Mechanism of Fingolimod?
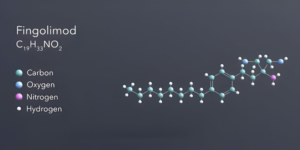
Fingolimod’s mechanism of action in treating relapsing-remming multiple sclerosis (MS) is complex but involves its interaction with specific molecules in the body. Here’s a breakdown:
Sphingosine-1-Phosphate (S1P): These are naturally occurring signalling molecules involved in various cellular processes, including immune cell movement.
S1P Receptors: Cells have receptors on their surface that bind to S1P, triggering specific actions. Fingolimod doesn’t directly target S1P, but it interacts with these receptors.
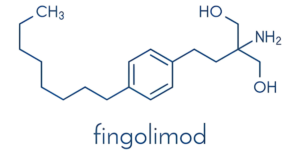
Lymphocyte Sequestration: Fingolimod gets converted to an active form inside the body. This active form binds to several S1P receptors (particularly S1P1, S1P3, S1P4) on lymphocytes (immune cells). This binding causes the receptors to be internalized and degraded by the cell, essentially removing them from the cell surface.
Reduced Lymphocyte Migration: Without these S1P receptors, lymphocytes are less responsive to S1P signals that normally direct their movement out of lymph nodes and into the bloodstream. Consequently, fingolimod keeps lymphocytes sequestered within lymph nodes, reducing their ability to migrate to the central nervous system and contribute to MS inflammation.
What Class of Drug is Fingolimod?
Fingolimod belongs to a specific class of medications known as sphingosine 1-phosphate receptor modulators (S1PRMs). These drugs act by targeting specific molecules in the body called sphingosine 1-phosphate receptors (S1PRs).
S1PRs are found on the surface of various cell types, including immune cells. They play a crucial role in regulating various cellular functions, particularly the movement and activity of immune cells.
What are the Uses of Fingolimod?
Fingolimod’s primary therapeutic use lies in treating relapsing-remitting multiple sclerosis (RRMS). RRMS is a specific subtype of MS characterized by episodes of worsening symptoms (relapses) followed by periods of partial or complete recovery.
How Fingolimod Helps in RRMS:
Fingolimod doesn’t cure MS, but it can significantly impact the course of the disease by:
Reducing Relapse Frequency: Studies have shown that fingolimod can substantially decrease the number of relapses experienced by RRMS patients.
Slowing Disability Progression: Fingolimod may help slow down the worsening of disability associated with MS, potentially improving patients’ quality of life.
How to Use Fingolimod Tablet?
Fingolimod tablets are a prescription medication used to treat relapsing-remitting multiple sclerosis (RRMS). Here’s a breakdown of the proper way to take fingolimod tablets:
Dosage Form:
Fingolimod comes as a tablet to be swallowed whole.
Dosage Schedule:
Fingolimod tablets are typically taken once daily, with or without food.
Your doctor will determine the exact dosage specific to your individual needs.
Directions for Taking:
Wash your hands with soap and water before handling the tablet.
Remove the tablet from the blister pack using dry hands.
Swallow the tablet whole. Do not crush, chew, or break the tablet.
You can take fingolimod with or without food. If it upsets your stomach, taking it with food may help.
What are the Side Effects of Fingolimod Tablet?
Fingolimod tablets, like many medications, can cause side effects. While not everyone experiences them, it’s important to be aware of the possibilities. Here’s a breakdown of some common and more serious side effects:
Common Side Effects:
Headache: This is a frequent side effect, often occurring in the initial stages of treatment.
Back pain, pain in arms or legs: These can occur and may improve over time.
Stomach pain, diarrhea: Fingolimod can sometimes cause digestive issues.
Flu-like symptoms: Fever, chills, cough, and stuffy nose may be experienced.
Increased liver enzymes: Routine blood tests will monitor for this potential side effect.
Serious Side Effects:
Slow heart rate (bradycardia): This is a potential risk, especially with the first dose. Monitoring is crucial.
Allergic reactions: Skin rash, itching, hives, or swelling of the face, lips, tongue, or throat require immediate medical attention.
Liver injury: Symptoms like nausea, vomiting, loss of appetite, yellowing of skin or eyes, or unusual weakness/fatigue might indicate liver problems. Seek medical attention promptly.
Increased risk of infections: Fingolimod can weaken the immune system, making you more susceptible to infections.
Macular edema (eye swelling): Vision changes require prompt evaluation by an ophthalmologist.
What are the Warning and precautions of Fingolimod Tablet?
Fingolimod tablets are a powerful medication for relapsing-remitting MS, but their use comes with certain warnings and precautions. Here’s a breakdown of key information to consider:
Before Taking Fingolimod:
Allergy: Don’t take fingolimod if you have a known allergy to it or any of its ingredients.
Medical Conditions: Inform your doctor about any pre-existing medical conditions, especially heart problems (slow heart rate, arrhythmias), liver disease, eye issues (macular edema), or a weakened immune system.
Medications: Disclose all medications you take, including prescriptions, over-the-counter drugs, vitamins, and herbal supplements, as fingolimod can interact with some medications.
Pregnancy and Breastfeeding: Fingolimod can harm an unborn baby and is not recommended for pregnant or breastfeeding women. Discuss alternative treatment options with your doctor if you plan to become pregnant.
During Treatment:
Monitoring: Regular doctor visits and blood tests are crucial while taking fingolimod to monitor for potential side effects like slow heart rate, liver problems, or increased infection risk.
Vaccinations: Discuss vaccinations with your doctor before starting fingolimod, as it may affect your immune response to vaccines.
Infections: Be mindful of hygiene practices and inform your doctor promptly if you experience any signs of infection (fever, chills, etc.).
Vision Changes: Report any changes in vision to your doctor immediately, as fingolimod can increase the risk of macular edema.
Additional Precautions:
Driving and Operating Machinery: Fingolimod may cause dizziness or fatigue, so exercise caution when driving or operating machinery.
Alcohol Consumption: Alcohol can worsen some fingolimod side effects. Discuss alcohol consumption with your doctor.
How Does Fingolimod Interact with Other Medicines?
Fingolimod tablets can interact with other medications, potentially affecting their effectiveness or increasing the risk of side effects. Here’s why understanding these interactions is crucial:
How Interactions Occur:
Fingolimod is metabolized (broken down) by the body through an enzyme system. Certain medications can either inhibit or induce this enzyme system, impacting fingolimod’s breakdown and potentially leading to higher blood levels.
Fingolimod can also affect how other medications work by influencing their absorption, distribution, or elimination from the body.
Medications to Avoid or Use with Caution:
Medications that slow heart rate (bradycardia): Beta-blockers, digoxin, and certain calcium channel blockers can worsen fingolimod’s potential for slowing the heart rate.
Medications for irregular heartbeat: Some medications used for arrhythmias can further increase the risk of heart rhythm problems with fingolimod.
Immunosuppressants: Fingolimod itself suppresses the immune system and combining it with other immunosuppressants may heighten the risk of infections.
Can Kidney Patients Take Fingolimod Tablet?
Fingolimod tablets are a treatment option for relapsing-remitting MS, but kidney function is a crucial factor to consider. Here’s a breakdown of the potential risks and why consulting a healthcare professional is essential.
Reduced Kidney Function:
Fingolimod is eliminated from the body primarily through the kidneys. If your kidney function is already compromised, fingolimod may not be effectively removed from your system. This can lead to a buildup of the drug in the body, potentially increasing the risk of side effects.
Potential Consequences:
Increased Side Effects: Higher fingolimod levels may lead to a more intense experience of common side effects or even trigger more serious ones.
Monitoring Challenges: Regular monitoring of blood levels and potential side effects becomes even more critical with reduced kidney function.
Can Liver Patients Take Fingolimod Tablet?
The liver plays a vital role in processing and eliminating medications from the body. Fingolimod is metabolized (broken down) by the liver. If your liver function is already compromised, fingolimod may not be processed effectively. This can lead to a buildup of the drug in the system, potentially increasing the risk of side effects.
Potential Concerns for Liver Patients:
Increased Liver Enzyme Levels: Fingolimod can cause elevated liver enzymes, even in healthy individuals. This effect might be more pronounced in patients with pre-existing liver problems.
Liver Injury: In rare cases, fingolimod has been linked to more serious liver damage. This risk is particularly concerning for those with pre-existing liver disease.
Monitoring Challenges: Regular monitoring of liver function becomes even more crucial for patients taking fingolimod, especially if they have underlying liver issues.
Does fingolimod Cause Weight Gain?
The fingolimod has limited evidence for direct weight gain
Clinical Studies: Weight gain wasn’t reported as a side effect in clinical trials of fingolimod. This suggests it may not directly cause weight gain in most people.
Focus on Other Factors: Changes in weight during MS can be influenced by various factors, including reduced mobility due to disease progression or changes in appetite caused by steroid medications used for MS flares.
Potential Indirect Effects:
Fluid Retention: Fingolimod can sometimes cause fluid retention, which may lead to a slight increase in body weight on the scale. This isn’t actual fat gain but temporary water weight.
Increased Appetite: Some people experience an increase in appetite while taking fingolimod. This could contribute to weight gain if dietary habits and exercise levels aren’t adjusted accordingly.